By Patrick Conway, M.D., principal deputy administrator and chief medical officer, CMS; and Tim Gronniger, deputy chief of staff, CMS
The unfortunate experience of having to return to the hospital after recently being treated—or watching the same thing happen to a friend or family member—is all too common. Potentially avoidable hospital readmissions that occur within 30 days of a patient’s initial discharge are estimated to account for more than $17 billion in Medicare expenditures annually.[1] Not only are readmissions costly, but they are often a sign of poor quality care. Many readmissions can be avoided through improvements in care, such as making sure that patients leave the hospital with appropriate medications, instructions for follow-up care, and follow-up appointments scheduled to make sure their recovery stays on track.
To address the problem of avoidable readmissions, the Affordable Care Act created the Hospital Readmissions Reduction Program, which adjusts payments for hospitals with higher than expected 30-day readmission rates for targeted clinical conditions such as heart attacks, heart failure, and pneumonia. The Centers for Medicare & Medicaid Services has also undertaken other major quality improvement initiatives, such as the Partnership for Patients, which aim to make hospital care safer and improve the quality of care for individuals as they move from one health care setting to another.
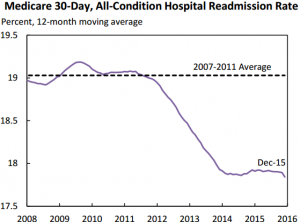
The data show that these efforts are working. As described below, between 2010 and 2015, readmission rates fell by 8 percent nationally. Today, CMS is releasing new data showing how these improvements are helping Medicare patients across all 50 states and the District of Columbia. The data show that since 2010:
- All states but one have seen Medicare 30-day readmission rates fall.[2]
- In 43 states, readmission rates fell by more than 5 percent.
- In 11 states, readmission rates fell by more than 10 percent.
Across states, Medicare beneficiaries avoided almost 104,000 readmissions in 2015 alone, compared to if readmission rates had stayed constant at 2010 levels. That means Medicare beneficiaries collectively avoided 104,000 unnecessary return trips to the hospital. Cumulatively since 2010, the HHS Assistant Secretary for Planning and Evaluation estimates that Medicare beneficiaries have avoided 565,000 readmissions.
The Hospital Readmissions Reduction Program is just one part of the Administration’s broader strategy to reform the health care system by paying providers for what works, unlocking health care data, and finding new ways to coordinate and integrate care to improve quality. Other initiatives include Accountable Care Organizations, as well as efforts by Quality Improvement Organizations and Hospital Engagement Networks, which fund quality improvement expert consultants to work with provider and hospital communities to improve care. The goal of all of these efforts is to spend our health care dollars more wisely to promote better care for Medicare beneficiaries and other Americans across the country.
| State | 2010 | 2015 | % Change in Readmission Rates | Reduction in readmissions in 2015 compared to 2010 | ||
| Hospital Admissions | Readmission Rate | Hospital Admissions | Readmission Rate | |||
| AK | 9,809 | 14.50% | 9,954 | 13.70% | -5.50% | -78 |
| AL | 154,856 | 17.20% | 143,210 | 16.20% | -5.80% | -1,503 |
| AR | 103,056 | 17.70% | 92,562 | 16.60% | -6.20% | -993 |
| AZ | 135,293 | 16.60% | 128,061 | 14.80% | -10.80% | -2,270 |
| CA | 574,176 | 17.60% | 547,558 | 16.60% | -5.70% | -5,580 |
| CO | 83,346 | 14.20% | 81,822 | 12.90% | -9.20% | -1,099 |
| CT | 109,888 | 18.10% | 96,492 | 16.70% | -7.70% | -1,306 |
| DC | 23,907 | 20.00% | 23,194 | 18.50% | -7.50% | -346 |
| DE | 29,827 | 17.40% | 32,257 | 15.60% | -10.30% | -575 |
| FL | 619,368 | 18.20% | 588,187 | 17.70% | -2.70% | -3,161 |
| GA | 209,500 | 17.50% | 191,485 | 16.20% | -7.40% | -2,453 |
| HI | 16,824 | 14.90% | 15,799 | 12.90% | -13.40% | -315 |
| IA | 100,490 | 15.50% | 91,256 | 14.50% | -6.50% | -910 |
| ID | 25,432 | 12.50% | 28,139 | 12.20% | -2.40% | -78 |
| IL | 421,395 | 19.80% | 335,610 | 17.40% | -12.10% | -8,108 |
| IN | 210,919 | 17.40% | 186,241 | 16.10% | -7.50% | -2,474 |
| KS | 90,545 | 16.30% | 87,224 | 14.70% | -9.80% | -1,361 |
| KY | 162,249 | 19.70% | 132,511 | 17.90% | -9.10% | -2,384 |
| LA | 129,123 | 18.70% | 112,328 | 16.90% | -9.60% | -2,013 |
| MA | 208,356 | 19.00% | 197,649 | 17.90% | -5.80% | -2,213 |
| MD | 189,323 | 21.10% | 170,510 | 18.90% | -10.40% | -3,789 |
| ME | 43,450 | 16.10% | 38,571 | 15.50% | -3.70% | -232 |
| MI | 343,346 | 18.60% | 280,152 | 18.00% | -3.20% | -1,767 |
| MN | 129,642 | 15.70% | 130,725 | 14.60% | -7.00% | -1,435 |
| MO | 203,685 | 18.20% | 174,677 | 16.90% | -7.10% | -2,311 |
| MS | 106,281 | 19.10% | 96,252 | 17.60% | -7.90% | -1,469 |
| MT | 27,962 | 13.90% | 27,518 | 13.10% | -5.80% | -231 |
| NC | 269,108 | 17.00% | 235,283 | 15.90% | -6.50% | -2,472 |
| ND | 26,562 | 15.40% | 26,650 | 14.40% | -6.50% | -267 |
| NE | 60,007 | 15.70% | 56,791 | 14.40% | -8.30% | -735 |
| NH | 36,189 | 15.70% | 39,871 | 15.30% | -2.50% | -152 |
| NJ | 281,282 | 20.30% | 250,924 | 17.60% | -13.30% | -6,774 |
| NM | 36,209 | 15.20% | 33,016 | 14.80% | -2.60% | -118 |
| NV | 51,787 | 18.00% | 52,308 | 17.00% | -5.60% | -529 |
| NY | 491,897 | 19.90% | 402,439 | 17.80% | -10.60% | -8,407 |
| OH | 325,091 | 18.80% | 267,743 | 16.80% | -10.60% | -5,405 |
| OK | 119,346 | 17.40% | 106,073 | 15.60% | -10.30% | -1,878 |
| OR | 58,182 | 14.30% | 61,393 | 14.20% | -0.70% | -75 |
| PA | 369,418 | 18.10% | 324,166 | 16.60% | -8.30% | -4,995 |
| RI | 24,142 | 19.00% | 24,705 | 17.00% | -10.50% | -487 |
| SC | 130,950 | 16.50% | 125,993 | 15.50% | -6.10% | -1,237 |
| SD | 31,269 | 14.90% | 30,806 | 13.20% | -11.40% | -515 |
| TN | 207,875 | 18.40% | 180,666 | 16.80% | -8.70% | -2,905 |
| TX | 571,147 | 17.10% | 509,738 | 16.10% | -5.80% | -4,960 |
| UT | 33,534 | 12.20% | 38,142 | 11.50% | -5.70% | -261 |
| VA | 207,241 | 17.50% | 211,674 | 16.40% | -6.30% | -2,302 |
| VT | 15,439 | 15.30% | 16,332 | 15.40% | 0.70% | 21 |
| WA | 130,798 | 15.30% | 131,817 | 14.20% | -7.20% | -1,388 |
| WI | 137,336 | 15.60% | 124,274 | 14.50% | -7.10% | -1,373 |
| WV | 70,144 | 19.90% | 60,630 | 18.60% | -6.50% | -777 |
| WY | 13,277 | 15.10% | 12,838 | 14.20% | -6.00% | -110 |
[1] Jencks, S. F., Williams, M. V. and Coleman, E. A. (2009). ‘Rehospitalizations among patients in the Medicare fee-for-service program’. New England Journal of Medicine, 360 (14), 1418-1428. [2] The readmission rate in Vermont was virtually unchanged, increasing slightly from 15.3% in 2010 to 15.4% in 2015. This change correlates to 21 additional readmissions compared to if the state’s rate had remained constant.